The Transforming Episode Accountability Model (TEAM) is the Centers for Medicare & Medicaid Services’ (CMS) newest mandatory value-based care alternative payment model, launching in January 2026 and running through December 2030. TEAM is designed to increase a hospital’s accountability around episode costs and quality with a specialized focus across high-cost, high-volume surgical episodes. TEAM continues CMS’s long-term strategy to tie reimbursement to measurable outcomes and cost efficiency for all Medicare patients.
For hospitals and health systems, TEAM represents a significant milestone in the evolution of bundled payments that will reward organizations that can effectively manage episode costs, minimize complications, and deliver consistently high-quality, patient-centered care.
Understanding the Transforming Episode Accountability Model (TEAM)
The Transforming Episode Accountability Model is a five-year, episode-based payment program that holds hospitals financially accountable for both the cost and quality of care provided during specific 30-day surgical episodes. It is mandatory for more than 700 hospitals nationwide, including acute care, safety net, rural, Medicare-dependent, sole community, and essential access community hospitals located in designated Core-Based Statistical Areas (CBSAs).
What surgical episodes are included in TEAM?
TEAM includes several high-volume and high-cost surgical procedures:
- Lower Extremity Joint Replacement (LEJR)
- Surgical Hip/Femur Fracture Treatment (SHFFT)
- Spinal Fusion
- Coronary Artery Bypass Graft (CABG)
- Major Bowel Procedures
By bundling payments around these procedures, CMS aims to create consistent incentives for hospitals to coordinate care, avoid preventable complications, and manage costs across the entire surgical recovery period.
How TEAM Measures Hospital Performance
Hospital performance under the Transforming Episode Accountability Model is based on two primary metrics:
- Total Medicare Fee-for-Service (FFS) Spending compared to discounted target price
- Quality Performance measured across standardized clinical and patient-reported outcomes (PROs)
Hospitals that deliver care more efficiently than their benchmark and achieve strong quality scores are eligible for positive reconciliation payments. Conversely, organizations that exceed target costs or underperform on quality metrics may owe CMS repayments.
What quality measures are included in TEAM?
Over the course of the five-year model, CMS will evaluate hospitals across multiple performance measures, as shown below:
%20Quality%20Measures.png)
Each measure contributes to a hospital’s Composite Quality Score (CQS), which adjusts the final reconciliation amount. High-quality performance can increase financial gains, while lower scores can amplify losses.
TEAM Participation Tracks and Risk Exposure
CMS has established three distinct participation tracks within the Transforming Episode Accountability Model (TEAM), each defining a hospital’s level of financial risk and reward. All hospitals begin in Track 1 unless they opt to begin in Track 3; after PY1, Tracks 1 and 2 are reserved for specific hospital types:
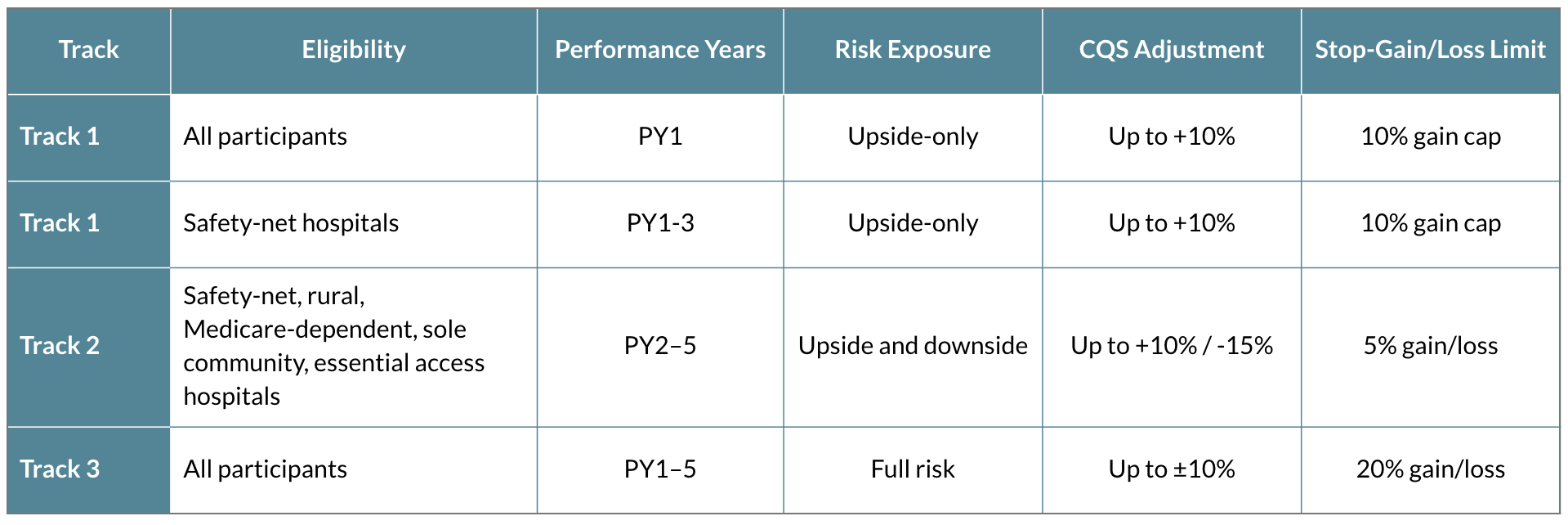
This tiered approach allows hospitals with less experience in bundled payment models to begin with lower risk exposure before advancing toward more comprehensive financial accountability.
The Quality-to-Payment Connection: Composite Quality Score (CQS)
The Composite Quality Score (CQS) is central to TEAM’s design. It consolidates multiple performance measures into a single score, adjusting hospital payments according to overall quality.
- High CQS: Yields greater upward adjustment or smaller reductions to reconciliation payments.
- Low CQS: Results in steeper reductions or higher repayment obligations.
This direct linkage ensures that quality improvement is not only clinically beneficial but financially advantageous. To produce the CQS, each performance measure is scaled based on national percentiles, then weighted by the number of patient episodes attributed to the participating hospital.
New Care Coordination Requirements
In support of CMS’s goal to have all Medicare and most Medicaid beneficiaries under an accountable care relationship by 2030, TEAM introduced a new primary care referral requirement. Hospitals must provide each beneficiary a referral to a primary care provider upon or before discharge, ensuring continuity of care after the anchor hospitalization.
Failure to comply can trigger CMS audits, corrective action plans, or reductions in TEAM payments. This highlights CMS’s intent to extend accountability beyond the hospital walls and into the continuum of post-acute care.
4 Common Challenges Hospitals Face Under TEAM
While the Transforming Episode Accountability Model (TEAM) framework creates clear pathways to improved value, it also introduces operational challenges that demand strategic preparation.
- Variation in Care Plans
- Challenge: Inconsistent protocols and lack of standardization lead to unpredictable outcomes and cost variability.
- Solution: Leverage digital tools to standardize evidence-based care pathways across surgeons and facilities while emphasizing patient-level personalization.
- Low PROMs Capture Rates
- Challenge: Hospitals must achieve at least 50% matched pre-op and 1-year post-op PROMs collection for all eligible THA/TKA patients to fulfill the THA/TKA PRO-PM requirements. Additionally, the Information Transfer PRO-PM must be completed for a specified number of patients.
- Solution: Automate PROMs collection, integrate reminders, and educate patients on the purpose and impact of these surveys.
- Limited Patient Adherence
- Challenge: Patients who disengage post-surgery often experience complications that extend episodes and drive costs.
- Solution: Deploy digital education, remote monitoring, and proactive outreach to sustain engagement throughout the recovery process.
- Manual Data Collection Burden
- Challenge: Manual PROMs and data collection and reporting drains staff resources and increases risk of non-compliance as well as manual errors, potentially risking patient safety.
- Solution: Implement platforms that automatically collect, format, and submit outcome data to CMS registries and quality programs, and establish broad and standardized workflows for data collection.
How Does Force Therapeutics Enable TEAM Success?
Force Therapeutics helps hospitals align with the Transforming Episode Accountability Model by digitizing the patient journey, automating data collection and reporting, and improving clinical efficiency across every stage of the surgical episode. By implementing Force, hospitals reduce preventable complications, eliminate unnecessary post-op care steps while preserving those recommended by the care team, and meet PRO-PM requirements.
Reduce 30-Day Readmissions
- Remote Monitoring and Smart Alerts: Passively collect data on a continuous basis, identifying early warning signs to prevent complications.
- Actionable Watchlists: Enable proactive outreach to at-risk patients.
- Comprehensive Education: Deliver gold-standard education to support patients in recognizing and managing symptoms before they escalate.
Shorten Length of Stay and Promote Home Discharge
- Real-Time Communication: Provide patients with answers to their questions quickly through direct messaging, and enable them to share wound images or exercise videos, ensuring safe home recovery and reducing patient anxiety.
- Pre-Op Preparation: Ensure patients have clear and accurate expectations ahead of surgery and recovery, increasing confidence and readiness for discharge.
Lower Post-Acute Care Costs
- Virtual Rehab and Wound Management: Replace costly home health visits with guided self-care.
- Automated Check-ins: Gather recovery data and flag potential complications.
Automate Outcomes Data Collection
- PROMs Automation: Send time-based forms and reminders to sustain high response rates.
- Registry Integration: Streamline submission to AJRR and CMS quality reporting programs.
How Should Hospitals Prepare for TEAM Implementation?
Hospitals should be actively preparing to meet the requirements of the Transforming Episode Accountability Model, which starts in January 2026. Key preparation steps include:
- Conduct a baseline analysis across cost, readmissions, SNF utilization, PROMs collection, and other cost and quality measures. Hospitals should keep in mind that the performance period for quality measures in PY1 already elapsed on June 30th 2025. This means TEAM hospitals can currently only impact quality performance for PY2 and beyond.
- Establish standardized surgical pathways and integrate evidence-based content across sites.
- Adopt a digital patient engagement platform to automate personalized patient education and data reporting.
- Train care teams on CMS metrics, documentation requirements, and reconciliation methodologies.
- Engage executive sponsors and quality leaders to oversee multidisciplinary readiness efforts.
By proactively aligning infrastructure, workflows, and patient engagement strategies, hospitals can mitigate risk and position themselves for financial success under TEAM.
The Road Ahead
The Transforming Episode Accountability Model reflects CMS’s broader vision for a fully accountable, outcomes-driven health system by 2030. Hospitals that adapt early and embrace digital patient engagement, automated outcomes collection, and standardized care delivery will not only comply with TEAM but emerge as leaders in value-based surgical care.
Force Therapeutics is proud to partner with hospitals and health systems preparing for TEAM success, offering proven tools to improve patient outcomes, reduce costs, and streamline compliance across the surgical episode.
Book a consultation on TEAM with Force Therapeutics:



.webp)


