The Centers for Medicare & Medicaid Services (CMS) has finalized its FY 2026 Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital Prospective Payment System (LTCH PPS) rule. Most key updates proposed to the Transforming Episode Accountability Model (TEAM) in the proposed rule have been finalized without any changes. Below is a summary of some of the most important updates; the full final rule can be found in the federal register.
To learn more about TEAM, here’s a comprehensive guide designed for orthopedic care teams. You can also listen to a recent panel discussion featuring expert orthopedic surgeons and executives from Geisinger and Newton-Wellesley Hospital as they explore cost accounting, remote patient engagement, care coordination, PROMs collection, and more.
Information Transfer PRO-PM
One of the key updates to TEAM in this final rule is the addition of the Information Transfer Patient Reported Outcome-based Performance Measure (Information Transfer PRO-PM) as a new quality measure for all TEAM outpatient episodes in performance years 3-5. This quality measure captures patient feedback on how well care teams communicated and coordinated information during transitions, focusing on the patient perspective in measuring care quality, and encouraging hospitals to enhance communication during care transitions, especially post discharge.
To ensure compliance, hospitals will have to administer this one-time 9 question survey between 2-7 days after a procedure. They will also have to submit that data through the Hospital Quality Reporting system, either directly or through a vendor. Learn how Force Therapeutics can help your organization seamlessly comply with the Information Transfer PRO-PM by effectively preparing your patients for surgery and recovery through high-quality remote education that keeps patients well informed of their recovery plan throughout the episode of care.
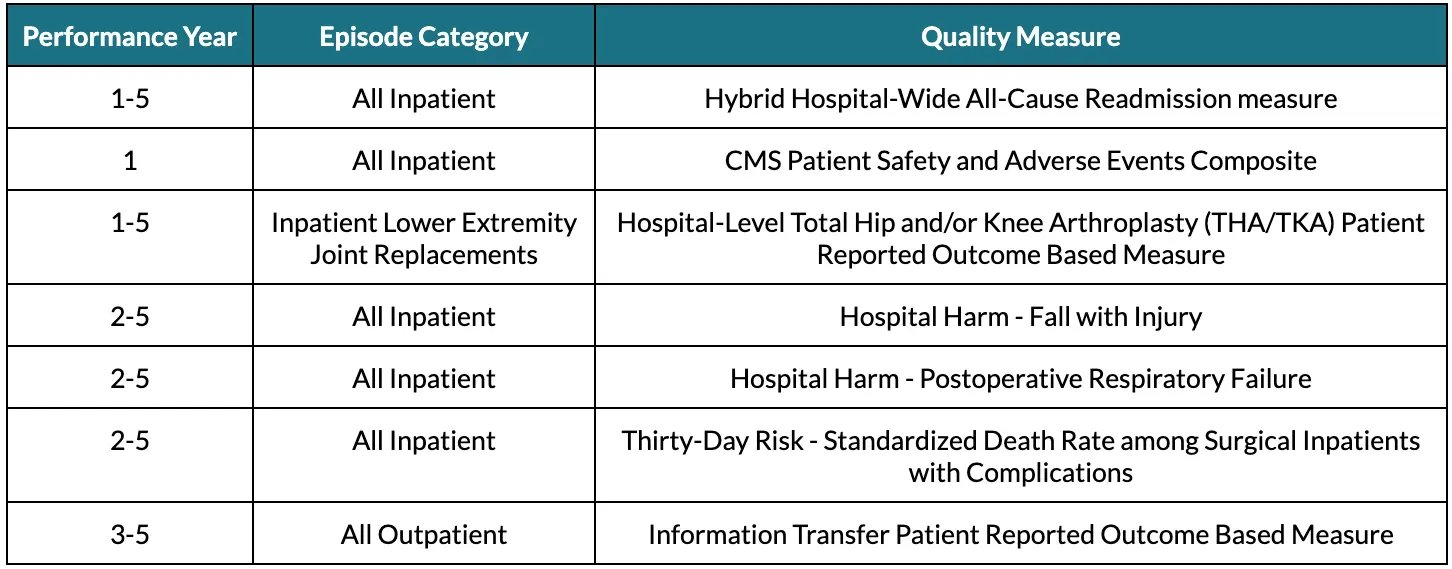
The table below, featured in the CMS IPPS and LTCH PPS final rule, shows the various quality measures required under TEAM, by performance year.
Hybrid Hospital-Wide Readmission (HWR) Measure
CMS had designed the quality measures of TEAM to align with measures that were already in place under other programs, such as the Hospital Inpatient Quality Reporting (IQR) program, to avoid placing additional reporting burdens on TEAM hospitals. In late 2024, CMS had extended the timeline for reporting the core clinical data elements and linking variables for the Hybrid HWR under the IQR program; this would have impacted TEAM hospitals because it would have misaligned the timelines for the Hybrid HWR between the IQR and TEAM.
However, in this final rule, CMS finalized a policy to maintain alignment by utilizing only the claims portion (without inclusion of the core clinical data elements and linking variables) of the Hybrid HWR measure to calculate TEAM composite quality score. Subsequent TEAM performance years will utilize the complete Hybrid HWR Measure.
Low-Volume TEAM Episodes and Lack of Quality Measure Performance Data
Not all TEAM hospitals perform large volumes of each TEAM episode category. In this final rule, TEAM hospitals that do not meet the low-volume threshold of 31 episodes (of a given category) in a baseline period would not be held accountable for any episode spending that exceeds the target price for the relevant episode category.
In addition, for TEAM hospitals that have no or incomplete raw quality measure scores for a given quality measure, CMS will assign a “neutral” scaled quality measure score of 50 points, representing the midpoint of the quality score scale. While this still means that a hospital's composite quality score–which impacts annual reconciliation–will be negatively affected by missing or incomplete data, it reduces the impact of having insufficient quality data on overall reconciliation to some extent.
Primary Care Service Referrals
As part of TEAM, hospitals are required to refer patients to primary care services on or prior to discharge. In this final rule, CMS modified the language surrounding this requirement to clarify that TEAM participants must refer patients to the same established primary care provider recorded on the patient’s admission to hospital or outpatient department. If no such provider is recorded, TEAM participants must include a new referral to a primary care provider as part of discharge planning.
Additional Updates
As part of this final rule, the requirements for submission of health equity plans, reporting of social drivers of health data, and requirements for decarbonization and resilience initiatives have all been removed from TEAM. While some of these elements were previously set as voluntary requirements, CMS contends that the removal of these items from TEAM will reduce the overall administrative burden on participating hospitals.
Additionally, CMS has finalized its proposal to allow TEAM participants to use the TEAM skilled nursing facility (SNF) 3-day rule waiver for patients “discharged to hospitals and critical access hospitals (CAHs) providing post-acute care under swing bed arrangements”.
Looking Ahead
Ultimately, CMS finalized most of its proposals without any major changes. As the beginning of TEAM in January 2026 approaches, participating hospitals should be laser focused on ensuring processes, care workflows, and internal stakeholders are prepared to ensure success under TEAM.
Force Therapeutics can help your organization with quality reporting and post-acute care resource utilization. Book a demo to learn how:

.webp)

.webp)


