The rapid shift to consumerism continues to accelerate as patients become more empowered to make decisions about their own care. In the past, healthcare stakeholders were each siloed in their specific role, cultivating gaps in communication and care and leading to frustrated consumers. Now, collaboration between providers, patients, caregivers, administrators, payers, technology companies, and regulators will be essential to achieve the highest level of patient satisfaction. This evolution of healthcare is commonly referred to as “patient centricity”.
In this new paradigm, patients have become the center of the care team. They are empowered to raise concerns, ask questions, make buying decisions, and proactively take charge of their recovery.
A competitive patient-centric model requires consumers of healthcare to have access to a tool for meaningful interactions at strategic points throughout their episode of care. It is critical for health systems to establish a structural framework for collaboration to cultivate trust and loyalty between care teams and the patients they serve.
The accelerated demand for quality care intensified when the pandemic hit, sending shock waves through the healthcare industry. It halted patients' access to typical care routines and forced health systems to transition from traditional in-person visits to a virtual setting, nearly overnight. Now, patient-centered care has never been more necessary, requiring healthcare providers to adapt to new norms; starting with a virtual care solution.
The emerging ecosystem of consumerism, expectations for individualized care, and regulations for patient-centered software and products are the major contributors to the need for organizations to formulate and swiftly adopt patient-centric models.
We have put together this data-backed guide to explain what a successful patient-centric strategy should encompass, the multitude of benefits and how to execute your plan.
Here is an overview of what we will cover:
1. What is patient centricity in healthcare?
2. Benefits of a patient centricity care approach
3. How to plan and implement a patient centric strategy
What is patient centricity in healthcare?
The current state of the healthcare industry is notoriously frustrating for patients. Not only are out-of-pocket costs extremely high, but it's also fairly common to experience additional issues tacked onto the bill such as: navigating insurance coverage, dealing with multiple points of contact for one procedure, communication barriers, long travel time, the list goes on…
Now, due to COVID and the historical issue of inconvenience for patients, the industry is making strides towards a new norm, which is a patient-centric approach to care, that perfectly compliments the evolution of consumerism in healthcare.
Evolution of Telehealth Reimbursement
But why are healthcare systems so quick to adapt to these changes? For one, many reimbursements models are now requiring value-based care, which advocates for patient satisfaction in a way like never before. In 2020, CMS released new rules for reimbursement when it comes to telehealth.
According to Centers for Medicare and Medicaid Services, prior to this waiver, Medicare could only pay for telehealth on a limited basis; When the person was receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or specified types of medical facilities for the service.
Now under the new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country, in addition to the patient’s places of residence, at the same rate as the traditional in-person visit.
Shortly after, an abundant number of commercial payers like Aetna and Blue Cross Blue Shield adopted plans that mirror the CMS reimbursement models.
Types of virtual services eligible for reimbursement
Here are a list of services eligible for reimbursement, declared and updated in 2021 by CMS.
Benefits of a Consumer-Centric Care
Decreased last-minute surgery cancellations
Reducing surgery cancellations are critical to hospitals because operating rooms and time slot scheduling must take place well in advance of the surgery. Cancellations close to or on the date of surgery means that the blocked operating room slot likely cannot be filled, which costs the hospital money.
Cancellations can occur for common reasons that are unavoidable, like if a patient becomes sick or has an emergency. However, these most often occur because patients have not been "optimized" appropriately. If there are not pre-operative office visits after surgery is scheduled, medical clearances or social needs (having a caregiver or a ride home from surgery) may not be completed, and the patients are not fully prepared for surgery. The medical team is forced to cancel the surgery when the patient arrives because it is not safe to proceed.
How to reduce surgery cancellations:
A digital tool can help reduce cancellation rates by:
- Augmenting in-office visits
- Reinforcing the steps to take before surgery through consistent education and reminders
- Easier communication with the care team to ensure that they are mentally and physically prepared for surgery
To put this to test, we analyzed Dartmouth-Hitchcock from the point of onboarding with our platform, and saw 8 surgeries cancelled out of 293 cases, which is a cancellation rate of ~ 2.7% after implementing Force Therapeutics.
According to this abstract by NCBI, the average cancellation rate is 14%. The data suggest that most cancellations occur because of administrative or structural processes that are potentially preventable. Targeting these processes with virtual tools can help to reduce cancellations for elective surgeries and thereby improve economic efficiency and patient outcomes.
Shortened hospital length of stay and same-day discharge enablement
For providers, CMS is encouraging site neutrality, giving them the option to decide where to perform procedures, with reimbursement rates in ambulatory surgery centers (ASCs) increasing by 2.7% in 2020.
It is imperative that during the shift to same day discharge, patient safety and satisfaction is not hindered. With less time in the hospital setting, adequate patient preparation is critical to ensure a successful and safe discharge. Technology can be utilized to scale preoperative education and optimization efforts.
When patients arrive for surgery, they should fully understand anesthesia, medications, discharge instructions, and how to communicate with their care team as needed. By providing consistent educational content in a rapid and absorbable way, patients can be optimized and prepared for same day discharge.
Exhibit
The outpatient setting for joint replacement, compared to the inpatient setting, is beneficial for patients with higher satisfaction from recovering at home, and comparable or lower complication rates (ER visits, Readmissions, Revision Surgeries).
However, this leaves providers with less face-to-face interaction with patients, requiring a multidisciplinary redesign to maintain patient safety and outcome quality.
The purpose of this whitepaper is to showcase how Northside Hospital utilizes technology to support their same day discharge program, and analyze patient reported outcome data trends between the hospital and ASC setting.
Reduction in readmissions and ED visits
Patients’ access to an online PT portal play a big role in decreasing the need for additional care and readmission followed by post-acute rehabilitation costs, without forfeiting patients’ postoperative functional outcomes at a healthcare organization.
With that being said, providers need to consider technological alternatives to formal PT in order to successfully reduce post-acute costs in a bundle.
Exhibit
In this study, Geisinger felt the pressure to institute a virtual solution for managing remote patients in rural settings, and to adhere to the bundled payment model.
With 60-70% of all joint replacement patients falling within a 120-day episode bundle (pre-op through post-op), Geisinger was at clinical and financial risk for what happened outside their facility. Demonstrating reduced costs in readmissions and unnecessary traditional outpatient services within the 90-day period after surgery was critical.
Given limited in-house resources, Geisinger realized they could no longer achieve their high standards of patient care without a more comprehensive, streamlined approach to managing patients in the home.

Workforce optimization and avoidance of hiring additional employees
Not only are we navigating a global pandemic, but now healthcare professionals are experiencing severe burnout. Healthcare systems near are far are running on fumes with depleted hiring budgets and staff shortages, with the demand for quality, individualized care looming over their heads.
A consumer-centric virtual care tool extends care management, and gives care teams and providers their valuable time back. It offers a unique opportunity to improving patient satisfaction by enhancing connectivity across surgeon teams while still reducing call volume.
With AI, a patient's journey will be unique to their care plan, configured by their provider, and backed by ample historical data collected from previous successful outcomes.
For example, our patient care platform has 3 main problem-oriented features that dynamically adjust remote patient care:
- Master care plan -- a singular pathway per procedure type (TKA, THA, shoulder recon, etc.)
- Configurable rules -- user-inputted, predetermined rules based on patient health data (BMI, demographic, sex, etc.) and treatment specifications (type, location, surgeon, etc.)
- Rules-based engine -- algorithm that uses configurable rules to dynamically adjust the master care plan on a per-case basis
Exhibit
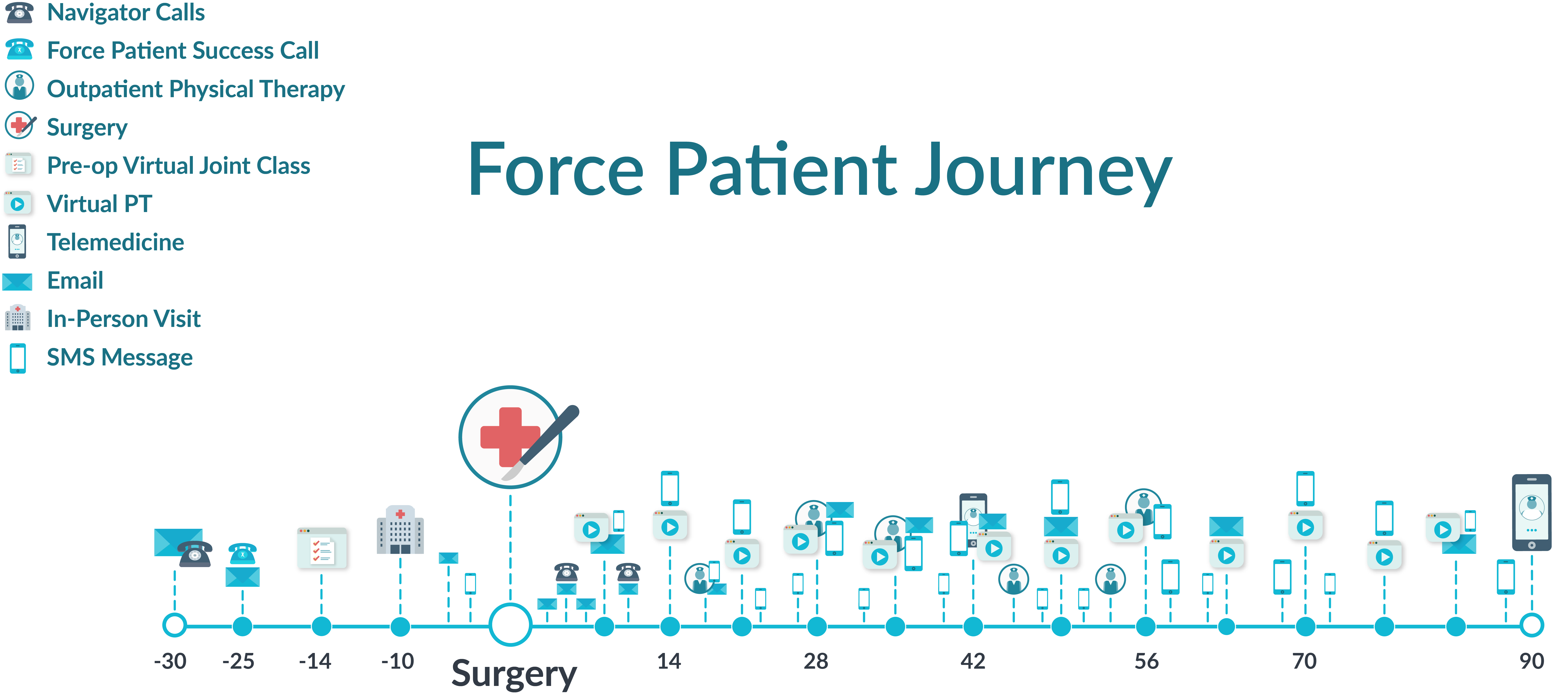
Here is a look into what a typical Force patient journey will look like, and every touchpoint they will receive pre-op, and throughout their post-op 90-day recovery plan.
Improved PROs collection rate and research enablement
Collecting patient reported outcomes efficiently and effectively as PROs become a mandatory part of the value-based care equation is the key to program success.
More importantly, the data you collect should be high-quality, in order to identify and address care gaps, and inform future care pathways for patient satisfaction and outcomes. By standardizing and automating collection, and providing research teams to support yours.
Patient satisfaction and market differentiation growth
In this digital age, consumerism relies heavily on online reviews, so having a patient-centric approach that improves patient experience and drives them to review their physicians online is an efficient way to give your organization a competitive edge.
In order to grow your market share in healthcare means bolstering your hospital’s reputation by building a strong online presence, paired with happy patients to back it up with real experiences and positive reviews. Establishing a strong brand reputation is the most effective way to grow your reach and build trust with potential patients looking for the high-quality care providers.
How to implement a patient centric strategy
1. Personalized care
It is important that patient care plans are crafted to benefit patient needs and circumstance. Individualized care ensures that patients are learning and recovering in optimal conditions for them, which can drastically improve patient outcomes and satisfaction.
2.Access to communication
Ensuring patients have access to care teams and providers is especially crucial in telehealth situations. Patient communication tools such as message capabilities can reduce call volume, while simultaneously extended clinicians’ and care teams’ reach. Patients care able to ask questions, request information, and voice concerns on their own terms.
3.Affordable care
Several patient centric care practices have been linked to lower patient and health systems costs, such as:
- Implementing virtual patient education classes
- Remote monitoring mitigating readmissions and unnecessary visits
- Same day discharge procedures
4.Education
Patient education is a huge factor in patient centric care and is the foundation for a patient’s care journey. By offering intelligent pro-op education, patients are more prepared for their procedures and are able to take an active role in their own recovery. This often results in improved patient reported outcomes, higher patient satisfaction rates, and more efficient recovery journeys.
Frequently Asked Questions:
What is patient-centric care?
Patient centric care is a type of care model that focuses on the patient experience in a multifaceted approach which redesigns care plans to cater to patients as individuals, focusing on patient success and satisfaction. This care model is holistic and addresses patient care from a multitude of angles to ensure a high quality, low cost, short recovery, care journey that can be adaptable to patients’ needs.
Why is patient centricity important?
This type of care model is a way to tract how patients are preforming in surgery, how they’re recovering, and even how well they’re interacting with online education systems. Tracking this information year-over-year is a way to show grow in patient outcomes and satisfaction, with can be valuable when building hospital reputation and/or achieving Center of Excellence status.
What is patient centricity in pharma?
A notable example of patient centricity within the pharmaceutical space is the fight against the current opioid pandemic. It is important that pharma invest in patient-focused research relevant to current threats or dangers within the industry, such as opioid sparing. Investing in research for the purpose of alleviating systemic threats against patients is an excellent step towards patient centric care.
How can I be patient centric?
A crucial first step to patient centricity is ensuring that your health system is making business decisions with the patient as the focal point. Especially in larger health systems, patient should be top of mind when developing policy, calculating pricing, deciding protocols, etc. This helps to ensure that care systems are transparent and patient focused.
How does a patient-centric model work?
There are several attributes that patient centric care follows including access to care teams, patient engagement, pricing transparency, patient education, and intelligently integrative care teams & EMRs.
What is a patient-centric approach?
Value based care is a strong example of a patient centric approach that has growing studies proving its effectiveness. The value based care model focuses on quality of care administered to ensure patients are receiving the best possible outcomes.
What is value-based care?
Value-based care models revolve around the patient's treatment and how well healthcare providers can improve their quality of care based on certain metrics, such as:
- Reducing hospital readmissions
- Improving preventative care
- Using certified health technology
- Improving patient outcomes
Enable Your Organization for Success
Without the use of technology and AI, it is impossible to achieve or exceed the modern standard of patient-centricity in healthcare. Force Therapeutics’ platform give providers the power to make educated decisions for the betterment of their patient, increasing patient satisfaction, and reducing the burden of tact of cost for post-acute care.
This guide should have helped you understand, audit and evaluate what pieces are missing and the steps that need to be taken in order to become a completely patient-centric organization. The next step is to book a demo with us to discuss how our solution can enable your programs for vitality and growth.



